HBOT Safety/Review Questions #6
Which of the following are not allowed in the chamber?
A metal external fixator covered by 100% cotton wrap
A plastic E Collar covered by 100% cotton stockinette
A rubber stomach tube covered by a 100% cotton bandage
An IV catheter flushed, capped, and covered by a 100% cotton wrap
A cardiac holter monitor covered by a 100% cotton stockinette
ANSWER: 5. A cardiac holter monitor covered by a 100% cotton stockinette
The cardiac holter monitor is not allowed in the chamber even when covered in 100% cotton, because it is a device powered by a battery and is therefore a source of ignition and not permitted in the chamber. The overwhelming majority of fires occur when an external source of ignition is introduced into the chamber (Reference, Workman, WT, Hyperbaric Facility Safety, Best Publishing, 1999, page 488).
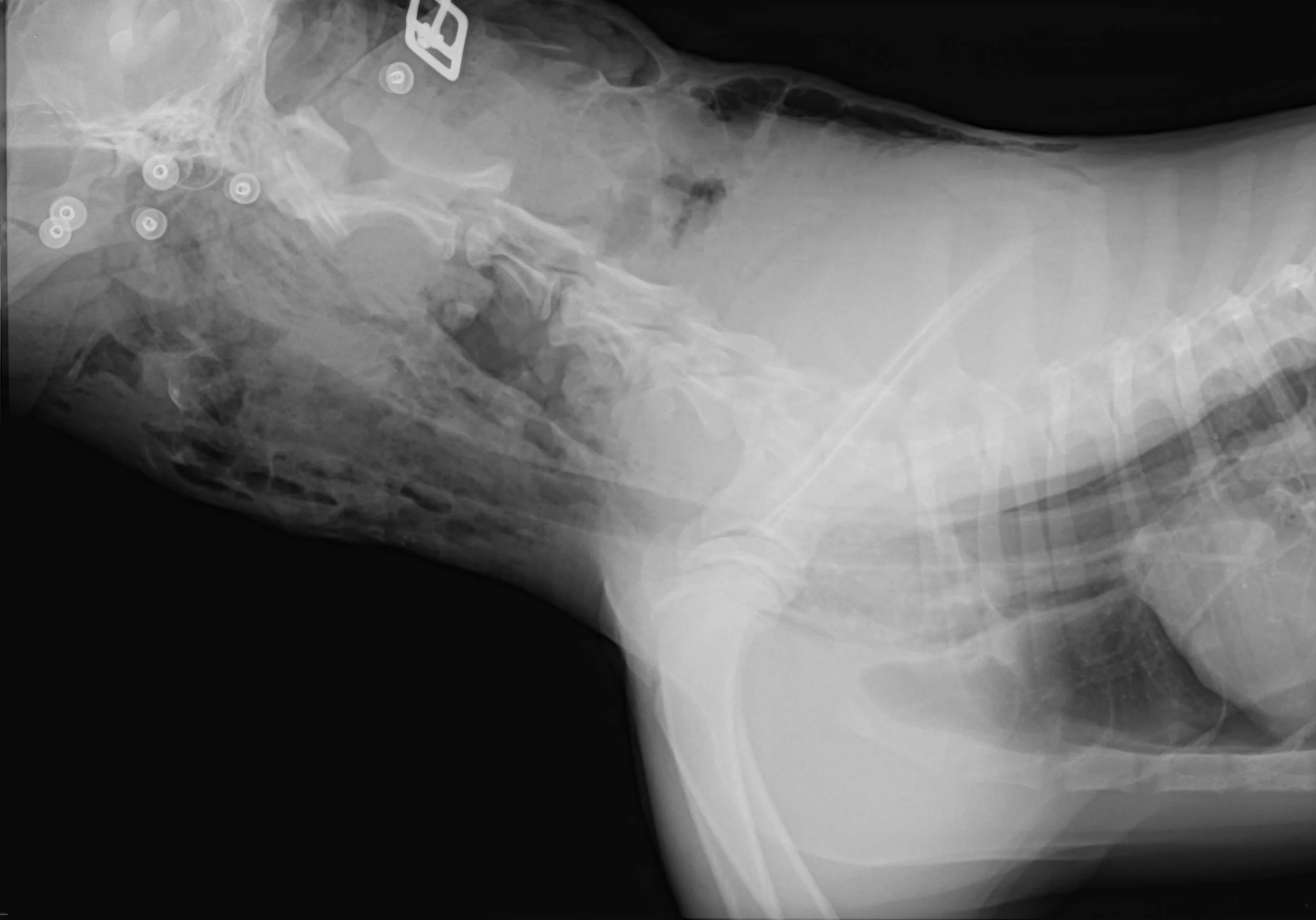
A canine is presented through the emergency and critical care servicer with a history of multiple shearing wounds resulting from injuries sustained from being hit and dragged by a car.
You take survey chest radiograph (above). Is this patient a candidate for adjuvant HBOT? Please discuss the reason(s) for your answer.
ANSWER: The radiograph reveals that this patient has extensive subcutaneous edema and pneumomediastinum. Progression to pneumothorax occurs in some patients with pneumomediastinum. It is not safe to treat a veterinary patient with pneumomediastinum in a monoplace HBOT chamber. If tension pneumothorax should develop while in the chamber, successful intervention might not be possible in a timely fashion. Untreated tension pneumothorax is an absolute contraindication for HBOT (Reference Jain, KK, Textbook of Hyperbaric Medicine Fifth and revised and updated Edition, Hogrefe, 2009, page 76).
The clinician should be aware that pneumothorax can result from causes other than blunt force trauma. For example, in humans it has been reported to result from the use of an air and water cooled turbine burr during a dental procedure (Reference, Shackelford D et al, Diffuse Subcutaneous Emphysema, Pneumomediastinum, and Pneumothorax AFter Dental Extraction. Ann Emerg Med, 1993 Feb; 22[2]: 248-50).
HBOT is a valuable adjuvant therapy in thermal burn care. Which species have been shown to benefit from adjuvant HBOT in thermal burn injury as published in peer reviewed publications?
rabbits
mice
guinea pigs
canines
ANSWER: All of the above.
Adjuvant HBOT has been found to be beneficial in the treatment of thermal burn wounds in rabbits, mice, guinea pigs, and canines. In fact, it has been shown to dramatically reduce hospitalization time and total treatment costs in humans as well. (Reference Cianci, P et al, Adjunctive Hyperbaric Oxygen Therapy in the Treatment of Thermal Burns, Journal of Undersea & Hyperbaric Medical Society, 2013, vol 40, no 1: 89-108). 20 of 22 studies in this report showed benefit for the use of HBOT for acute thermal injury, leading the AHA to designate thermal burn injury as a class IIa indication for HBOT in humans.
It has been demonstrated that the areas adjacent to third degree burns are hypoxic when compared to normal skin, and that the tissue oxygen levels in these areas can ONLY be raised by oxygen administered AT PRESSURE (Gruber, RP et al, Hyperbaric Oxygen and Pedicle Flaps, Skin Grafts, and Burns, Journal of Plastic and Reconstructive Surgery, 1970, 45: 24-30).
A client gives you a 100 % cotton garment and asks you to place it inside the chamber with her cat, who has been treated with adjuvant HBOT multiple times at your hospital to help manage severe chronic osteoarthritis.
You examine the garment and find a warm object in a pocket (images below). Please discuss how you would proceed in these circumstances.
ANSWER: The object is a hand warmer which uses lighter fluid as fuel. These are still available for purchase today, and represent the source of ignition in several human HBOT chamber fires (Reference, Workman, WT, Hyperbaric Facility Safety- A Practical Guide, Best Publishing, page 488). More contemporary hand warmers use chemical reactions to produce heat (pictures below).
All these items are prohibited in the chamber. However, experience in human HBOT clearly demonstrates that some people are unaware of the danger of potential combustion. Thus, when treating our veterinary patients we must be vigilant, and always follow protocol. Pay extra attention to those you are treating as outpatients. Prepare your patients using the same routine every time. The standard rule of thumb is...only the patient and 100% cotton are allowed in the chamber. If it is not cotton and it is on the patient (and permitted in the chamber), cover it with 100% cotton!
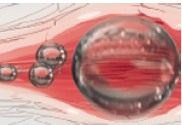
HBOT can be used to treat vascular, cerebral and pulmonary air embolism. Which of the following is a situation which can occasionally result in the development of air embolism?
Placing and using a central venous IV line
Performing an interventional procedure such as the placement of cardiac pacemaker
Performing a Caesarean section
Hydrogen peroxide use on an open wound or ingestion of hydrogen peroxide
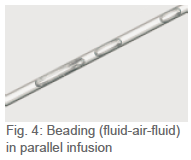
ANSWER: All of the above. (Reference Jain, KK, Textbook of Hyperbaric Oxygen Therapy, Hogrefe, 5th and revised Edition, pages 104-109). Air embolism will be increasingly recognized in veterinary medicine as more central venous lines and interventional procedures are performed, especially when parallel infusions are performed. In addition, pressure gradients in uterine sinuses favor the development of air embolism during C-Section. Finally, the use of hydrogen peroxide on open wounds or orally has also been associated with the development of air embolism (images below).
HBOT is the treatment of choice to shrink the size of the gas bubbles blocking blood flow in air embolism. Boyles Law describes this effect of pressure on reduction of gas volumes and thus bubble size.
A 6 year old poodle mix canine was found with traumatic injuries including pelvic fractures and signs of head and neck trauma. It appeared he had been hit by a car.
He was referred for adjuvant hyperbaric oxygen therapy. DMSO had been given intravenously to the patient prior to referral, and a neck bandage with a DMSO dressing had also been applied just prior to discharge from the referring hospital.
Please discuss two reasons why you cannot place this patient in the chamber with this dressing or with remnants of DMSO remaining on the hair coat and skin.
ANSWER: This patient cannot be placed in the chamber for an undetermined period of time, as DMSO is highly flammable (Reference MSDS, ScienceLab.com). In addition, this compound is a potent solvent to most acrylics and even some metals (Reference Atofina, Product Information from a DMSO manufacturer). Thus, both the intravenous and the topical DMSO represent a combustion hazard, and certain parts of the chamber may be damaged by exposure to this solvent. This question originates from an actual clinical case, and demonstrates the need for constant safety vigilance on the part of doctors and staff when considering the use of adjuvant HBOT.
You are treating a female spayed canine with marked azotemia and pyelonephritis. Urine culture by cystocentesis has revealed an organism susceptible only to gentamycin, which is being given IV.
You want to support GFR at all times. You are employing adjuvant HBOT, so you have the patient on intravenous fluids during her sessions. The patient was initially very depressed and moved about very little during her sessions.
She has progressively become much brighter and more active . Today during her HBOT session she was moving about her module, and she pulled her IV extension off where it inserts into the inside of the "pass through port" on the chamber door. The IV set on the outside of the door pops off, and oxygen begins escaping through the IV " pass through port" on the door.
Is this an emergency situation?
What actions should you take?
ANSWER: This is not an emergency situation. You should first insert a sterile catheter plug into the IV "pass through port" on the chamber door, and thus stop the flow of oxygen out of the chamber. (See image.)
You may then consult with the attending doctor and ask if it is appropriate to gradually end this HBOT session with a standard, slow decompresion over 10-15 minutes, then flush and reconnect the intravenous line connections and begin a new, abbreviated session to make up for the time remaining in the shortened session; or the doctor may decide to simply end this particular session and wait until the next scheduled HBOT session for this individual patient.
Elevation of the pO2 of ischemic tissue (by adjuvant HBOT) optimizes the antimicrobial activity of aminoglycosides such as gentamycin by facilitating transport of the drug through the cell membranes of bacteria (Reference , Kindwall and Whelan, Hyperbaric Medical Practice, Best Publishing, Second Edition Revised, 2004, page 224).
Which of the following drugs may increase the potential for oxygen toxicity induced seizures in the hyperbaric chamber?
enrofloxacin
penicillin
furosemide
prednisolone
ANSWER: 4. prednisone
Glucocorticoids such as prednisolone, prednisone, dexamethasone, triamcinolone, depomedrol, or methylprednisone may hasten the onset or increase the potential for oxygen induced seizures. Eleations in adrenocortical hormones in naturally occurring hyperadrenocorticism also decrease oxygen tolerance (Reference Kindwall and Whelan, Hyperbaric Medicine Practice, 2004, Best, page 76, and Jain, KK, Textbook of Hyperbaric Medicine, 5th Edition, Hogrefe, page 52).